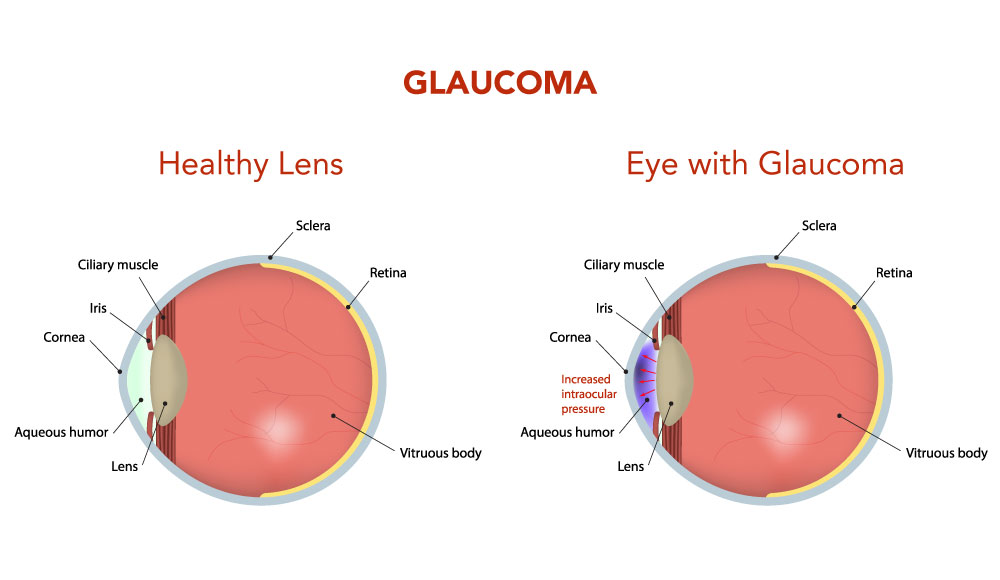
Chronic open-angle glaucoma
This is the most common type of glaucoma and develops very slowly.
In cases of chronic glaucoma, there are usually no noticeable symptoms because the condition develops very slowly. People don’t often realise their sight is being damaged because the first part of the eye to be affected is the outer field of vision (peripheral vision). Vision is lost from the outer rim of the eye, slowly working inwards towards the centre.
Changes in vision are often linked to getting older, which is why it is so important to have your eyes checked regularly. You should have an eye test at least every two years.
Primary angle-closure glaucoma
This is rare and can occur slowly (chronic) or may develop rapidly (acute) with a sudden, painful build-up of pressure in the eye.
Acute angle-closure glaucoma develops rapidly. Symptoms are often severe and may include:
- Intense pain
- Redness of the eye
- Headache
- Tender eye area
- Seeing halos or ‘rainbow-like’ rings around lights
- Misty vision
- Loss of vision in one or both eyes that progresses very quickly
As a result of these symptoms, some people may also feel sick or be sick. Symptoms of acute glaucoma are not constant. They can last for one or two hours before disappearing again. But each time the symptoms occur, your vision is damaged a little more. It’s important to seek medical attention if you have any of the above symptoms.
Secondary glaucoma
This mainly occurs as a result of an eye injury or another eye condition, such as uveitis (inflammation of the middle layer of the eye).
Secondary glaucoma is caused by other conditions, such as uveitis(inflammation of the middle layer of the eye). It can also be caused by eye injuries and certain treatments, such as medication or operations.
It’s possible for the symptoms of glaucoma to be confused with the symptoms of the other condition. For example, uveitis often causes painful eyes and headaches. However, the glaucoma may still cause misty vision and rings or halos around lights.
Developmental glaucoma (congenital glaucoma)
A rare but sometimes serious type of glaucoma which occurs in very young children, caused by an abnormality of the eye.
Recognising the symptoms of developmental glaucoma (also known as congenital glaucoma) can be difficult due to the young age of the baby or child.
However, your child may display symptoms, such as:
- Large eyes due to the pressure in the eyes causing them to expand
- Being sensitive to light (photophobia)
- Having a cloudy appearance to their eyes
- Having watery eyes
- Jerky movements of the eyes
- Having a squint, which is an eye condition that causes one of the eyes to turn inwards, outwards or upwards, while the other eye looks forward
Preventing glaucoma
Attending regular optician appointments will help to ensure any signs of glaucoma can be detected early and allow treatment to begin.